Sailing an ocean is a wonderful experience, but it also implies isolation. It implies a temporary lack of access to modern healthcare facilities and infrastructure. While it is indeed temporary, you do want to think ahead about different scenarios and plan. If you are so medically inclined, please proceed 🫱
As often is the case, the best way to start is to ask yourself some questions:
- What do I want to be able to do onboard?
- How do I get support?
- What can be done in terms of prevention?
- Who does what?
📋 What do I want to be able to do onboard?#
When creating your medical kit, you should reflect about the risks associated with the crossing and what you want to be able to do at sea. You clearly won’t be performing open heart surgery 🫀, but you do need to be able to deal with sea sickness 🤢. What about minor cuts, bigger cuts or potential fractures? Respiratory infections, traveller’s diarrhea or menstrual cramps?
You might be facing this question for the first time. How do you even know what you want to be able to do onboard? You should definitely read up on what is recommended, should also think about it yourself and consult with your doctor. And you should do this for several reasons: you naturally want to ensure everyone’s well-being. At the same time, the skipper/owner has an actual legal duty of care for the crew, and is ultimately accountable.
Fortunately, very thorough resources are available for preparations, several freely or for cheap. For instance:
- The Centre de Consultation Médicale Maritime (CCMM, in France) offers a very complete list for the suggested onboard pharmacy (⌘/control + F and then search for “Excel” here). Other national telemedical services provide their own information. Check them out, call them, and decide which option is best for you.
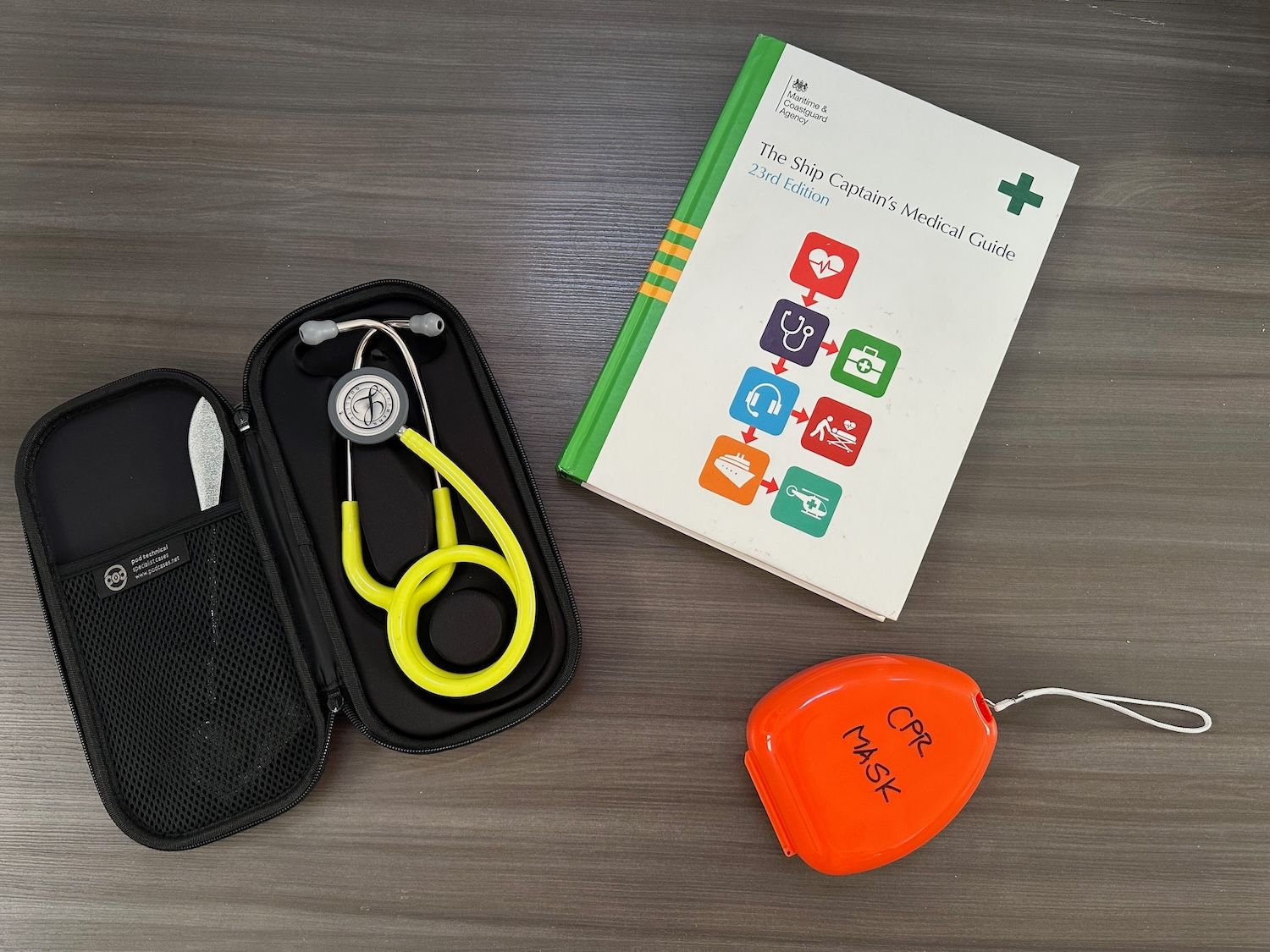
- The Ship Captain’s Medical Guide or equivalent should be a resource available on board to consult at any time. Peruse it, and you’ll find hints about what you should watch out for.
📞 Something happened. Who do I call and how do I call them?#
🏞️ National and private services#
According to the International Labour Organisation Convention of 2006 and the International Maritime Organisation, all maritime nations must have a centre that provides medical services for seafarers 24 hours a day. Nations have complied, albeit with different approaches: while Italy and Spain have created organisations specifically dedicated to providing telemedical services, other countries like France, Germany, and Sweden haved designated doctors employed in hospital units to provide this service. In addition, a number of private companies that offer these services also exist, often selling their own medical kit. SeaDoc and MSOS are two noteworthy examples, but several more exist. It’s worth doing your own research here. You will need to pre-register your intended trip with these companies and will be invoiced for the support offered.
☎️ How do you establish contact?#
Essentially, you need to think about your communications system here. VHF will only work if you’re close to shore. After that, calling or emailing are your options. We had a satellite phone as well as Starlink (meaning we could also do calls over Skype, if need be). It is important to brief your crew on how to contact the telemedical services in case of an emergency (and unblock any PIN-locked devices or share the PIN!).
🇫🇷 The French experience#
The French maritime telemedical assistance service (TMAS), called Centre de Consultations Médicales Maritimes (CCMM) was the natural choice for us. Inês speaks French fluently (although the CCMM staff also speak English), our boat is registered in France, and the service is offered free of charge. In addition, we found the following to be very helpful:
- The list of recommended medications to take onboard is freely available on their website;
- They publish clear instructions on how to establish contact and these work (Inês tested the numbers before departing, and they picked up the phone in less than 1 minute!);
- There is the possibility to pre-register your trip: Inês got in touch with the CCMM and shared the details of the boat, the planned itinerary, how many people would be onboard, along with their crew health forms, which the crew filled up beforehand.
- The CCMM asked for a the boat’s medical inventory. This ensures that they make suggestions based on what is available on the boat.
Fortunately, we did not require their services once at sea, although we did have to deal with a couple of medical situations.
🗝️ Prevention is key#
I cannot emphasize this enough. The best thing to do is to not have a problem in the first place. Put differently, Plan A is to never need to open your medical kit. Stay ahead of the problem. But how do you do that?
📆 Recommended appointments#
Before a big offshore cruising trip, you should meet with your general practicioner, to (1) control any chronic illnesses, (2) update vaccinations and (3) get the necessary prescriptions for the trip (always pack more than what you will need)! Discuss your sailing plans and whether you take any further particular care.
In addition, if travelling to tropical regions, you should schedule a travel medicine appointment. Here, you will discuss important points such as:
- The need for further vaccinations or a specific pharmacological prophylaxis (e.g., malaria)
- Talk about further prevention of infectious disorders:
- Which repellent should you buy? How should you use it?
- What can you eat and what should you avoid?
- What should you do in case of diarrhea or fever?
- Should you pack antibiotics? When should you take them?
These consultations can be very heavy in information. Fortunately, many national agencies offer freely available online resources. Check the CDC’s website, the Swiss Travel Medicine website, or your own country’s reading resources.
Thirdly, if you have 1 or more cardiovascular risk factors (>60 years, high blood pressure, smoker, obesity, diabetes), consider meeting with a cardiologist.
Finally, consider a dental check up and make sure you have good medical insurance: will they assist you if anything goes wrong? Do they cover a potential evacuation? Do they cover treatment/surgery in another country, if needed?
❤️ Safety culture#
About half of the medical problems on board are due to physical trauma. It is therefore well worthwhile to emphasize this aspect during your safety briefing (more on safety briefings in a later post). In particular, you should discuss the onboard hazards: the boom, winches, cleats, ropes, as well as cooking and the galley area.
Emphasize that you cannot cover every possible situation, but that the crew should think ahead. With that, certain principles become apparent:
- Handling winches with thumbs away from it
- Avoiding walking barefoot
- Not trying to contain sails or ropes with your bare hands
- Always being on the watch for potential hazards
- Looking after each other and speaking up ❤️
The latter point is particularly important during the crossing. Is someone showing clear signs of fatigue? Encourage them to sleep. Is someone getting sea sick? Help them prioritize getting better (and not feeling guilty!). Help folks stay hidrated… and so on 😊
😷 A word on pre-existing illnesses#
Many chronic conditions are well manageable nowadays, but it is the skipper’s and medic’s responsability to ultimately decide whether they wish to embark on an offshore passage with a specific person. As mentioned before, there is legal responsibility involved, but one should also note that, even with a person with a serious medical condition is happy to go, having a person with health problems can entail risk for the rest of the crew. In addition, rescue operations offshore are risky procedures. While we all strive to accommodate folks and be optimistic, a critical eye is necessary when it comes to this.
🩺 Training#
Not every boat can have a medical doctor on board, but every boat can have an informed crew trained in administering basic care, including first aid. Indeed, with the available communication options nowadays, you will probably reach a medical expert who can tell you what to do. But will you know how to do it? Training is useful to not only prevent disease, but also to prevent matters from escalating even further (i.e.,tertiary prevention). Many associations, companies and institutions offer training. This is well worthwhile booking in advance, as spaces are limited and these courses fill up fast!
🧑⚕️ Who does what?#
Every boat should have an assigned medic, if possible separate from the skipper. This is a highly specialized role, which should be taken on by the person with the most competence in the area. On Nuvem Mágica, Inês has a medical degree, and is therefore by default the medic. I took this responsibility very seriously. Here are some of the things I coordinated behind the scenes:
- Registering our crew with the CCMM
- Creating the medical kit from scratch, including:
- The first aid kit;
- The boat pharmacy
- Additional devices and aids (e.g., stethoscope, sphingomanometer, pulse oximeter)
- Evaluating the crew’s overall health
- Providing support to the crew with all things health (much of which was related to prevention, as per the section above)
If possible, assign a second medic. This person can not only provide support to the medic, but is also the pre-designated back up for the medic, should they become incapacitated.
🎒 Medical kits#
After all of this, I am sure you still want to know how to get an appropriate medical kit. Essentially, the right answer for you depends on the following factors:
- Size of the boat: space is limited, and you need to plan around constraints
- Pre-existing illness(es)
- National requirements from your boat’s flag
- Budget
In the end, there are two approaches. You either:
- Buy a pre-made kit (and maybe expand it);
- Or make one yourself.
Either way, do not forget to ensure you have a complete inventory which you can share with the telemedical services. While doing this, avoid commercial names when documenting things, and prefer the name of the active substance. Commercial names vary from country to country, whereas the name of the actual compound inside does not.
Finally, ideally store your kit in a visible spot or clearly signal where the medical kit is stored.
To conclude: medical preparations can be a dense topic. Therefore, it is well worth thinking ahead and starting to prepare early. If you feel any of this information or any of the resources are useful to you, let us know! A link on your own blog post or a tag on social media are much appreciated! It also helps us know whether we are on the right track or not.
Fair winds and healthy breezes 💨
Until our headings cross again,
Your Nuvem Mágica